Abstract
Background
The widespread use and success of allogeneic hematopoietic stem cell transplantation (allo-HSCT) can be affected by graft-versus-host-disease (GVHD), an immunological syndrome that involves tissue damage mediated by donor lymphocytes. Both, acute and chronic GVHD, result from an imbalance between the effector and regulatory arms of the immune system. On the other hand, worldwide, the main source of stem cells is peripheral blood (PBSC). However, its use has been associated with higher incidence of GVHD when compared with bone marrow. Although the fast engraftment using PBSC as a source of stem cells compares to that seen with G-CSF-primed bone marrow (G-BM), the latter, also associates with a decreased incidence of GVHD. At our institution, patients transplanted with G-BM, have a lower incidence of GVHD when compared to those transplanted with PBSC and steady state bone marrow (SS-BM). Some microenvironment characteristics of these sources of hematopoietic stem cells (HSCS) remain unknown, including differences between Tregs, Th17 cells, and cytokines, and its association with GVHD.
Aim
The aim of this study was to analyze lymphocyte subsets and associated cytokines in donor G-BM and SS-BM, comparing patients who developed GVHD and those who did not.
Material and Methods
A prospective analysis was performed in 48 donors SS-BM and G-BM collected from March 2002 to April 2017. Twenty two samples collected since March 2002 were thawed; since 2014, samples (20 mL) were immediately processed and analyzed. A 24 hour resting with RPMI, and posterior activation with PMA (50 ng/ml) for 48 hours was performed. Cells were harvested and cytokines were evaluated by flow cytometry (CBA assay).
From each sample, one million mononuclear cells were permeabilized, fixed, and stained with CD4-FITC, IL17A-PE, IFN -γ APC, and IL-4 PECy7, for their posterior phenotipication by flow cytometry. The samples were obtained in a BD LSR Fortessa cytometry, and analyzed with the Flow-Jo software. Comparison between variables was made by means of Student's t test using SPSS v.21.
Results
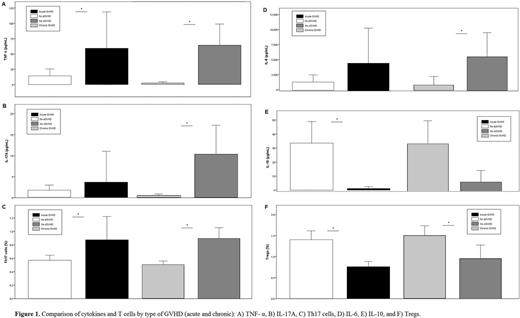
We found increased Tregs (1.46% ± 0.69 vs 1.01% ± 0.49, p=0.01) and Th2 (1.55% ± 0.36 vs 1.28% ± 0.39, p=0.02) subsets in G-BM compared to SS-BM. Nonetheless, although differences in cytokine production were observed, we did not find any statistical significance. Acute GVHD was diagnosed in 9% (n=3) and 20% (n=3) of patients receiving G-BM and SS-BM, respectively. Chronic GVHD was seen in 33% of patients in both groups (receiving SS-BM or G-BM). Thirty one patients did not present either GVHD. In all the cohort, indistinctively from the HSCs used, acute GVHD was characterized by a predominant pro-inflammatory profile, with increased TNFα (59.28 ± 56.6 vs 14.21 ± 36.2 pg/mL, p=0.011), and a higher percentage of Th1 (22.55% ± 4.8 vs 20.71% ± 4.8, p=0.04) and Th17 (0.87% ± 0.33 vs 0.57% ± 0.24, p=0.009) cells. Furthermore, a deficient suppressor response, with decreased IL-10 production (1.17 ± 1.26 vs 33.55 ± 49.3 pg/mL, p<0.0001) as well as lower Tregs percentage (0.76% ± 0.12 vs 1.40% ± 0.68, p<0.0001) was found. Likewise, chronic GVHD showed the same profile, but with more striking differences in pro-inflammatory cytokine production. The T cell subset profile in chronic GVHD also showed an imbalance between pro-inflammatory and suppressor subsets percentage ( figure 1 ).
Conclusions
This is the first study exploring the differences in T cells and cytokine profile between G-BM and SS-BM. Our results showed that G-BM has an enhanced suppressive phenotype compared to SS-BM. Also, patients who developed GVHD were characterized by an imbalance in pro-inflammatory and suppressor responses, with enhanced Th17 cells, as well as increased TNF-α, IL-6 and IL-17A production in contrast to a dampened Tregs frequency and IL-10 production which can explain the low frequency of GVHD in our transplanted patients using G-BM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal